Table of Contents
Opioids are drugs often prescribed to induce surgical anesthesia, relieve acute post-surgical pain, and treat other moderate to severe acute pain. When opioids are taken short-term and as prescribed, they can be effective and relatively safe. However, when misused or taken illegally, they present a high risk of addiction and overdose—and are the cause of the current healthcare epidemic in the United States.
BlueCrest Recovery offers substance abuse treatment in New Jersey for individuals struggling with opioid addiction. Our treatment center is staffed with experienced and compassionate professionals who understand this complex disease and its treatment. Contact our team online or call 888.292.9652 today to learn more about our opioid addiction treatment center in Woodland Park, NJ.
Understanding the Opioid Epidemic in the United States
 This is not the first epidemic of its kind the United States has faced. In the late 19th century, there was an epidemic of morphine addiction. It was not until the invention of heroin in 1898 that a new opioid appeared on the market and replaced morphine. It wasn’t long before doctors realized that it was far more dangerous than morphine, and they stopped prescribing it. However, when heroin became illegal, people were still addicted, and they turned to illicit opioids, which are even more dangerous. In the 1970s, opioid addiction rates started to rise in the United States—this time because of prescription opioids. Since then, the use and abuse of prescription opioids have only increased, leading to the current opioid epidemic.
This is not the first epidemic of its kind the United States has faced. In the late 19th century, there was an epidemic of morphine addiction. It was not until the invention of heroin in 1898 that a new opioid appeared on the market and replaced morphine. It wasn’t long before doctors realized that it was far more dangerous than morphine, and they stopped prescribing it. However, when heroin became illegal, people were still addicted, and they turned to illicit opioids, which are even more dangerous. In the 1970s, opioid addiction rates started to rise in the United States—this time because of prescription opioids. Since then, the use and abuse of prescription opioids have only increased, leading to the current opioid epidemic.
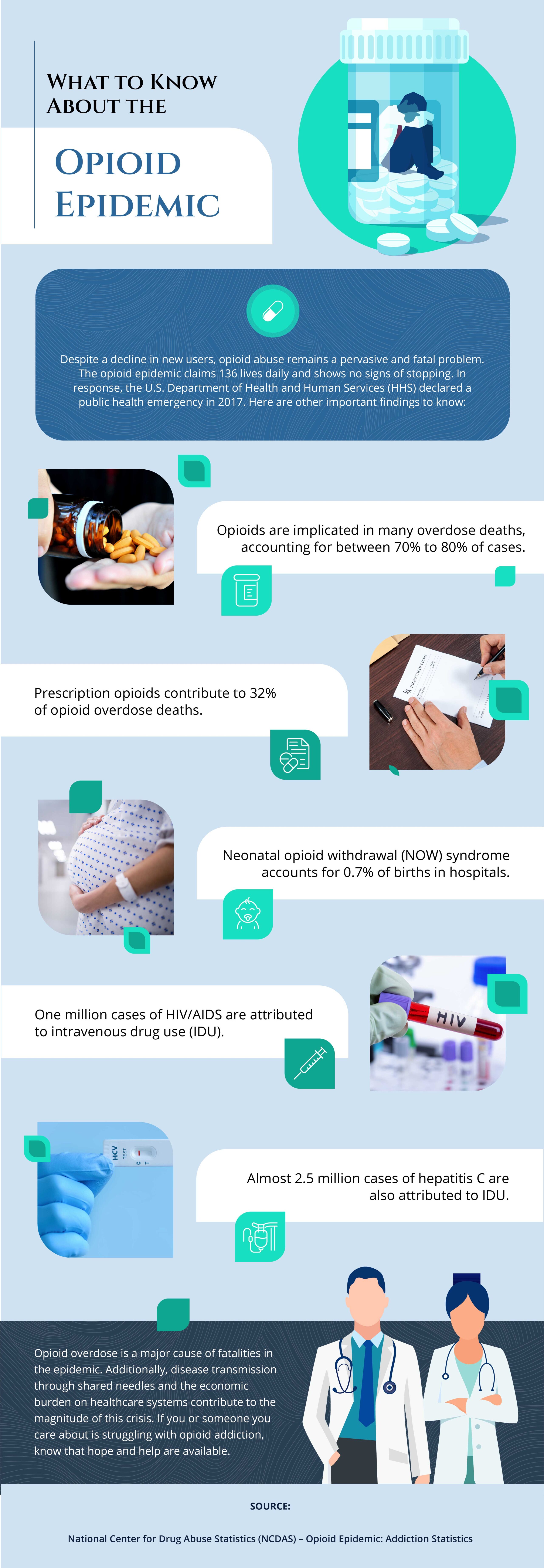
The opioid epidemic in the United States has been ongoing for over two decades, with a sharp increase in the number of deaths and hospitalizations linked to opioid misuse. According to the National Institute on Drug Abuse (NIDA), more than two million Americans suffer from substance use disorders (SUDs) related to prescription opioid pain relievers, and an additional 626,000 have an SUD related to heroin. Furthermore, over 130 people die every day from an opioid overdose.
Someone struggling with opioid addiction may misuse the following:
- Heroin
- Codeine
- Morphine
- Fentanyl
- Oxycodone
- Hydrocodone
The misuse of prescription opioids often leads to the use of heroin, a cheaper and more potent alternative. Misuse refers to taking medication in a manner or dose other than prescribed, taking someone else’s prescription, or taking it for the experience or feeling it causes. The NIDA reports that 80% of heroin users first misused prescription opioids.
Defining Opioids: What You Need to Know
Opioids are a class of drugs that bind to specific receptors in the brain and body for pain control. Its origins can be traced back to opium, which is derived from the poppy plant. Opioids are often used as prescription medications for pain relief. They work by blocking pain signals sent to the brain while also producing feelings of pleasure and relaxation. Opioids can also affect the reward center of the brain, leading to feelings of pleasure and euphoria. This effect can make the drugs addictive and dangerous if misused.
The opioid epidemic has cast much scrutiny on the frightening rise in opioid addiction and deaths in the last few decades. Consequently, physicians are becoming more cautious about prescribing opioids for conditions other than cancer pain, palliative care, and end-of-life comfort.
How Opioid Addiction Develops
Opioids send signals to the brain, spinal cord, and other areas of the body to increase relaxation and dull pain perception. The drugs also interact with the brain’s pleasure and reward center to increase dopamine levels and other chemicals, increasing feelings of pleasure, well-being, and euphoria. Although these same signals can be triggered naturally in the brain, opioids deliver the effects at a higher intensity, which can lead to drug addiction as users continually seek to repeat the effects. As opioid use continues, the brain adapts to the dose and demands more of the drug to produce the desired effect, leading to tolerance and addiction.
People most likely to develop an opioid addiction include individuals with a family history of substance abuse, those dealing with mental health conditions such as depression or anxiety, and people who have previously struggled with addiction to other substances.
The Risks of Opioid Abuse and Addiction
The misuse of opioids can lead to a range of harmful consequences, including:
Opioid addiction is a chronic condition that requires long-term management. Different treatment programs may be recommended based on an individual’s needs and level of addiction. At BlueCrest Recovery, our team works closely with individuals to create personalized treatment plans that address their unique needs and support them in achieving lasting long-term recovery from opioid addiction.
Recognizing the Symptoms of Opioid Addiction
Many physical, mental, and behavioral signs may warn of opioid abuse or addiction.
Behavioral Indicators of Opioid Addiction
Common behavioral changes may include:
- Taking higher doses than prescribed or more often than prescribed
- Stealing or forging prescriptions
- Requesting prescriptions from several different doctors
- Reporting a prescription as lost and ordering a new one
- Asking for early refills
Fluctuations in mood and energy levels, including rapidly swinging from high to low levels, can be a sign of opioid abuse, as can sleep disorders and risky behavior, including unprotected sex or injecting drugs.
Physical Symptoms of Opioid Addiction
The signs and symptoms of opioid abuse include:
- Constipation
- Nausea
- Feeling high (euphoria)
- Slowed breathing rate
- Drowsiness
- Confusion
- Poor coordination
- Increased dose required for pain relief
- Worsening or increased sensitivity to pain with higher doses
Older adults may be at a greater risk of adverse side effects from opioids, as they may take longer to metabolize drugs, take multiple prescriptions, and have other chronic diseases.
Opioid Overdose
Opioid overdose is a medical emergency. Signs of an overdose often include pinpoint pupils, unconsciousness, and respiratory depression. Other symptoms may include blue-tinged skin as a sign of poor circulation, an individual who is awake but unable to talk, choking sounds, an irregular pulse, and vomiting. If breathing becomes dangerously slow and shallow, too little oxygen may reach the brain, causing hypoxia. Hypoxia can lead to coma, brain damage, and death.
If you suspect an opioid overdose, contact emergency services immediately. If help arrives in time, naloxone can reverse the effects and prevent death. Most first responders now carry naloxone.


What Should You Expect from an Opioid Addiction Treatment Program?
Treating opioid addiction involves a multi-faceted approach that may include medical detoxification, therapy, and support groups. The specific treatment plan will depend on an individual’s needs and level of addiction. BlueCrest Recovery offers a comprehensive approach to treating opioid addiction, combining the following:
- Medication-assisted treatment (MAT)
- Individual therapy
- Group therapy
- Family therapy
- Aftercare planning and support services
The goal of treatment is to help individuals overcome the physical, mental, and psychological effects of opioid addiction and establish a strong foundation for lasting recovery. Our compassionate team works closely with each individual to provide personalized care and support every step of the way.
Get Started on Opioid Addiction Treatment in New Jersey at BlueCrest Recovery
BlueCrest Recovery takes a whole-person approach to treatment, considering not only a person’s physical needs but also their emotional, psychological, and spiritual needs. Contact our team online or call 888.292.9652 today to learn more about our approach to treatment in Woodland Park, NJ.




